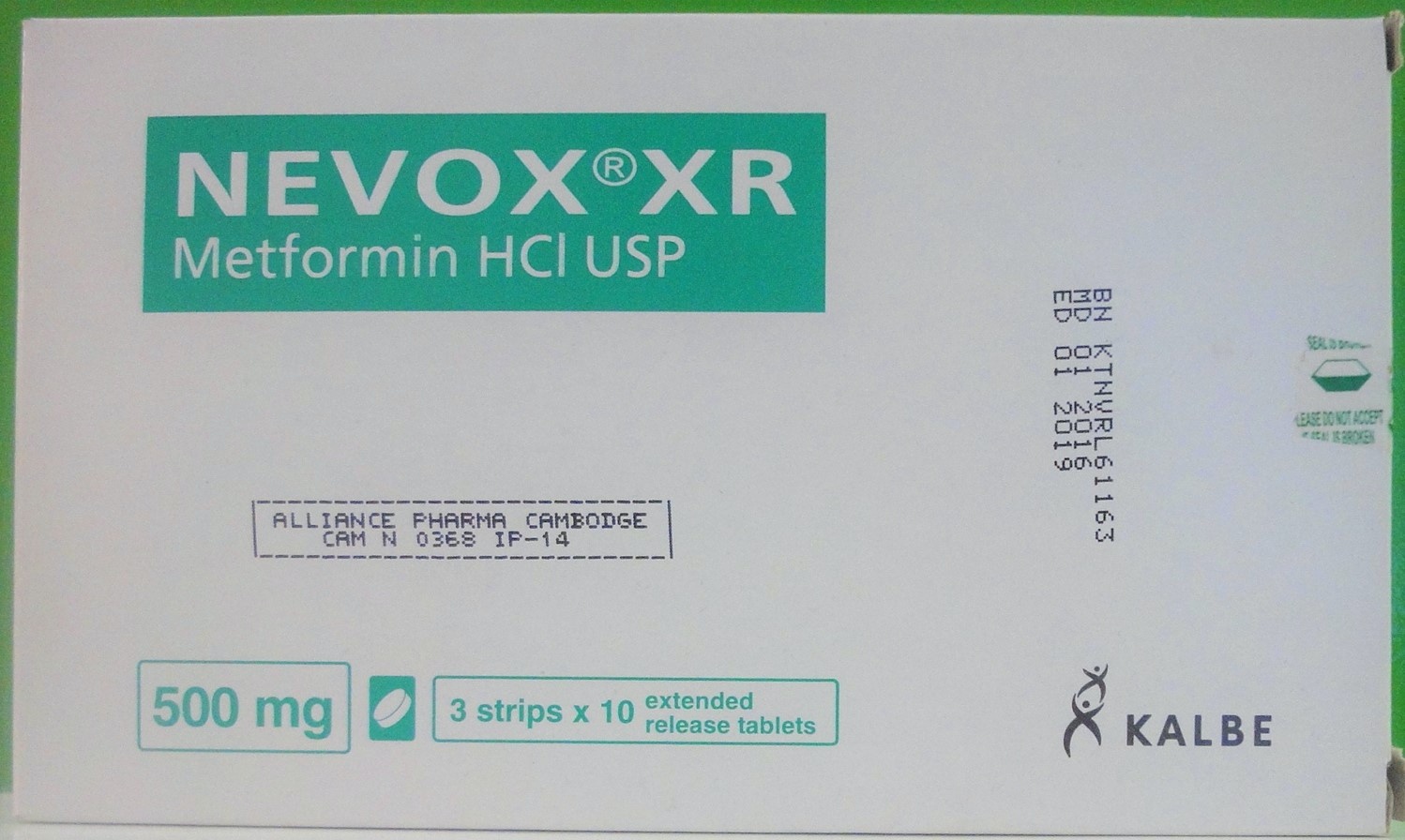
NEVOX XR Tablet
ក្រុមហ៊ុនផលិតឱសថ:
PT KALBE FARMA Tbk. Indonesia
ក្រុមហ៊ុនចែកចាយឱសថនៅប្រទេសកម្ពុជា:
ALLIANCE PHARMA CAMBODGE
- សារធាតុសកម្ម
- ប្រសិទ្ធិភាពព្យាបាល និង កម្រិតប្រើប្រាស់
- ហាមប្រើ
- ផលរំខាន
- អន្តរប្រតិកម្ម
- ស្ត្រីមានផ្ទៃពោះ និង ស្ត្រីបំបៅដោះកូន
- ការប្រុងប្រយ័ត្នជាពិសេស
- សកម្មភាពឱសថ បរិយាយប័ណ្ណឱសថ
-
សារធាតុសកម្ម
Metformin hydrochloride 500mg
-
ប្រសិទ្ធិភាពព្យាបាល និង កម្រិតប្រើប្រាស់
Indications
indicated in patients 17 years of age and older.
as monotherapy, are indicated as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes.
may be used concomitantly with a Sulfonylurea or Insulin to improve glycemic control in adults (17 years of age and older).
Dosage
There is no fixed dosage regimen for the management of hyperglycemia in patients with type 2 diabetes with this medicine or any other pharmacologic agent. Dosage must be individualized on the basis of both effectiveness and tolerance, while not exceeding the maximum recommended daily dose, this medicine should be started at a low dose, with gradual dose escalation, both to reduce gastrointestinal side effects and to permit identification of the minimum dose required for adequate glycemic control of the patient. During treatment initiation and dose titration, fasting plasma glucose should be used to determine the therapeutic response to this medicine and identify the minimum effective dose for the treatment. Thereafter, glycosylated hemoglobin should be measured at intervals of approximately three months. The therapeutic goal should be to decrease both fasting plasma glucose and glycosylated hemoglobin levels to normal or near normal by using the lowest effective dose of this medicine, either when used as monotherapy or in combination with Sulfonylurea or Insulin.
Monitoring of blood glucose and glycosylated hemoglobin will also permit detection of primary failure, i.e., inadequate lowering of blood glucose at the maximum recommended dose of medication, and secondary failure, i.e., loss of an adequate blood glucose lowering response after an initial period of effectiveness. Short term administration of this medicine may be sufficient during periods of transient loss of control in patients usually well-controlled on diet alone. This tablets must be swallowed whole and never crushed or chewed.
The maximum recommended daily dose in adults is 2000mg. This medicine should generally be given once daily with the evening meal.
Adults:
In general, clinically significant responses are not seen at doses below 1500mg per day. However, a lower recommended starting dose and gradually increased dosage is advised to minimize gastrointestinal symptoms. The usual starting dose is 500mg once daily with the evening meal. Dosage increases should be made in increments of 500mg weekly, up to a maximum of 2000mg once daily with the evening meal. If glycemic control is not achieved on 2000mg once daily, a trial of 1000mg twice daily should be considered.
Pediatrics:
Safety and effectiveness in pediatric patients have not been established. This medicine is not recommended in pediatric patients.
Transfer from other antidiabetic therapy
When transferring patients from standard oral hypoglycemic agents other than Chlorpropamide to NEVOX XR, no transition period generally is necessary. When transferring patients from Chlorpropamide, care should be exercised during the first two weeks because of the prolonged retention of Chlorpropamide in the body, leading to overlapping drug effects and possible hypoglycemia.
Concomitant with oral Sulfonylurea therapy in adult patients
If patients have not responded to four weeks of the maximum dose of this medicine monotherapy, consideration should be given to gradual addition of an oral prior primary or secondary failure to a Sulfonylurea has occurred.
With concomitant this medicine and Sulfonylurea therapy, the desired control of blood glucose may be obtained by adjusting the dose of each drug. However, attempts should be made to identify the minimum effective dose of each drug to achieve this goal. With concomitant this medicine and Sulfonylurea therapy, the risk of hypoglycemia associated with Sulfonylurea therapy continues and may be increased. Appropriate precautions should be taken. If patients have not satisfactorily responded to one to three months of concomitant therapy with the maximum dose of this medicine and the maximum dose of an oral Sulfonylurea, consider therapeutic alternatives including switching to Insulin with or without this medicine.
Concomitant and Insulin therapy in adult patients
The current Insulin dose should be continued upon initiation of NEVOX XR therapy. NEVOX XR therapy should be initiated at 500mg once daily in patients on Insulin therapy. For patients not responding adequately, the dose of this medicine should be increased by 500mg after approximately 1 week and by 500mg every week thereafter until adequate glycemic control is achieved. The maximum recommended daily dose is 2000mg for NEVOX XR. It is recommended that the Insulin dose be decreased by 10% to 25% when fasting plasma glucose concentrations decrease to less than 120mg/dl in patients receiving concomitant Insulin and NEVOX XR. Further adjustment should be individualized based on glucose-lowering response.
Specific patient populations
This medicine is not recommended for use in pregnancy. The initial and maintenance dosing of this medicine should be conservative in patients with advanced age, due to potential for decreased renal function in this population. Any dosage adjustment should be based on a careful assessment of renal function. Generally, elderly, debilitated, and malnourished patients should not be titrated to the maximum dose of this medicine. Monitoring of renal function is necessary to aid in prevention of lactic acidosis, particularly in the elderly.
-
ហាមប្រើ
1. Renal disease or renal dysfunction (e.g., as suggested by serum creatinine levels ≽1.5mg/dl (males), ≽1.4mg/dl (females) or abnormal creatinine clearance) which may also result from conditions such as cardiovascular collapse (shock), acute myocardial infarction, and septicemia
2. Congestive heart failure requiring pharmacologic treatment.
3. Known hypersensitivity to Metformin hydrochloride.
4. Acute or chronic metabolic acidosis, including diabetic ketoacidosis, with or without coma. Diabetic ketoacidosis should be treated with Insulin.
-
ផលរំខាន
Diarrhea led to discontinuation of study medication in 6% of patients treated with Metformin. Additionally, the following adverse reactions were reported in ≽1.0-≼5.0% of Metformin patients and were more commonly reported with Metformin than placebo: abnormal stools, hypoglycemia, myalgia, lightheaded, dyspnea, nail disorder, rash, sweating increased, taste disorder, chest discomfort, chills, flu syndrome, flushing, palpitation.
Diarrhea led do discontinuation of study medication in 0.6% of patients treated with Metformin. Additionally, the following adverse reactions were more commonly reported in ≽1.0-≼5.0% of Metformin extended-release than placebo: abdominal pain, constipation, distention abdomen, dyspepsia-heartburn, flatulence, dizziness, headache, upper respiratory infection, taste disturbance.
In clinical trials with Metformin in pediatric patients with type 2 diabetes, the profile of adverse reactions was similar to that observed in adults.
-
អន្តរប្រតិកម្ម
Interactions
Glyburide
In a single-dose interaction study in type 2 diabetes patients, co-administration of Metformin and Glyburide did not result in any changes in either Metformin pharmacokinetics or pharmacodynamics. Decreases in Glyburide AUC and Cmax were observed, but were highly variable. The single-dose nature of this study and the lack of correlation between Glyburide blood levels and pharmacodynamic effects, makes the clinical significance of this interaction uncertain.
Furosemide
A single-dose, Metformin-Furosemide drug interaction study in healthy subjects demonstrated that pharmacokinetics parameters of both compounds were affected by co-administration. Furosemide increased the Metformin plasma and blood Cmax by 22% and blood AUC by 15%, without any significant change in Metformin renal clearance. When administered with Metformin, the Cmax and AUC of Furosemide were 31% and 12% smaller, respectively, than when administered alone, and the terminal half-life was decreased by 32%, without any significant change in Furosemide renal clearance. No information is available about the interaction of Metformin and Furosemide when co-administered chronically.
Nifedipine
A single-dose, Metformin-Nifedipine drug interaction study in normal healthy volunteers demonstrated that co-administration of Nifedipine increase plasma Metformin Cmax and AUC by 20% and 9%, respectively, and increased the amount excreted in the urine, Tmax and half-life were unaffected. Nifedipine appears to enhance the absorption of Metformin. Metformin had minimal effects on Nifedipine.
Cationic drugs
Cationic drugs (e.g., Amiloride, Digoxin, Morphine, Procainamide, Quinidine, Quinine, Ranitidine, Triamterene, Trimethoprim, or Vancomycin) that are eliminated by renal tubular secretion theoretically have the potential for interaction with Metformin by competing for common renal tubular transport systems. Such interaction between Metformin and oral Cimetidine has been observed in normal healthy volunteers in both single-and multiple-dose. Metformin-Cimetidine drug interaction studies, with a 60% increase in peak Metformin plasma and whole blood concentrations and a 40% increase in plasma and whole blood Metformin AUC. There was no change in elimination half-life in the single-dose study. Metformin had no effect on Cimetidine pharmacokinetics. Although such interactions remain theoretical (except for Cimetidine), careful patient monitoring and dose adjustment of Metformin or Metformin extended-release and/or the interfering drug is recommended in patients who are taking cationic medications that are excreted via the proximal renal tubular secretory system.
Other
Certain drugs tend to produce hyperglycemia and may lead to loss of glycemic control. These drugs include the thiazides and other diuretics, corticosteroids, phenothiazines, thyroid products, estrogens, oral contraceptives, phenytoin, nicotinic acid, sympathomimetics, calcium channel blocking drugs, and isoniazid. When such drugs are administered to a patient receiving Metformin or Metformin extended-release, the patient should be closely observed for loss of blood glucose control. When such drugs are with-drown from a patient receiving Metformin or Metformin extended-release, the patient should be observed closely for hypoglycemia.
In healthy volunteers, the pharmacokinetics of Metformin and Propranolol, and Metformin and Ibuprofen were not affected when co-administered in single-dose interaction studies. Metformin is negligibly bound to plasma proteins and is, therefore, less likely to interact with highly protein-bound drugs such as Salicylates, Sulfonamides, Chloramphenicol, and Probenecid, as compared to the Sulfonylureas, which are extensively bound to serum proteins.
-
ស្ត្រីមានផ្ទៃពោះ និង ស្ត្រីបំបៅដោះកូន
This medicine is not recommended for use in pregnancy.
Teratogenic effects: Pregnancy category B
Recent information strongly suggests that abnormal blood glucose levels during pregnancy are associated with a higher incidence of congenital abnormalities. Most experts recommend that Insulin be used during pregnancy to maintain blood glucose levels as close to normal as possible.
Because animal reproduction studies are not always predictive of human response, Metformin of Metformin extended-release should not be used during pregnancy unless clearly needed. There are no adequate and well-controlled studies in pregnant women with Metformin or Metformin extended-release. Metformin was not teratogenic in rats and rabbits at doses up to 600mg/kg/day. This represents an exposure of about two and six times the maximum recommended human daily dose of 2000mg based on body surface area comparisons for rats and rabbits, respectively. Determination of fetal concentrations demonstrated a partial barrier to Metformin.
Nursing mothers
Studies in lactating rats show that Metformin is excreted into mild and reaches levels comparable to those in plasma. Similar studies have not been conducted in nursing mothers. Because the potential for hypoglycemia in nursing infants may exist, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. If Metformin or Metformin extended-release is discontinued, and if diet alone is inadequate for controlling blood glucose, Insulin therapy should be considered.
-
ការប្រុងប្រយ័ត្នជាពិសេស
Precautions
Monitoring of renal function
Metformin is known to be substantially excreted by the kidney, and the risk of metformin accumulation and lactic acidosis increases with the degree of impairment of renal function. Thus, patients with serum creatinine levels above the upper limit of normal for their age should not receive Metformin. In patients with advanced age, Metformin should be carefully titrated to establish the minimum dose for adequate glycemic effect, because aging is associated with reduced renal function. In elderly patients, particularly those ≽80 years of age, renal function should be monitored regularly and, generally, Metformin should not be titrated to the maximum dose. Before initiation of Metformin therapy and at least annually thereafter, renal function should be assessed and verified as normal. In patients in whom development of renal dysfunction is anticipated, renal function should be assessed more frequently and Metformin discontinued if evidence of renal impairment is present.
Use of concomitant medications that may affect renal function of Metformin disposition
Concomitant medication(s ) that may affect renal function or result in significant hemodynamic change or may interfere with the disposition of Metformin, such as cationic drugs that are eliminated by renal tubular secretion should be used with caution.
Intravascular contrast studies with iodinated materials can lead to acute alteration of renal function and have lactic acidosis in patients receiving Metformin. Therefore, in patients in whom any such study is planned, Metformin should be temporarily discontinued at the time of or prior to the procedure and reinstituted only after renal function has been re-evaluated and found to be normal.
Hypoxic states
Cardiovascular collapse (shock) from whatever cause, acute congestive heart failure, acute myocardial infarction and other conditions characterized by hypoxemia have been associated with lactic acidosis and may also cause prerenal azotemia. When such events occur in patients on Metformin therapy, the drug should be promptly discontinued.
Surgical procedures
Metformin therapy should be temporarily suspended for any surgical procedure (except minor procedure not associated with restricted intake of food and fluids) and should not be restarted until the patient’s oral intake has resumed and renal function has been evaluated as normal.
Alcohol intake
Alcohol is known to potentiate the effect of Metformin on lactate metabolism. Patients, therefore, should be warned against excessive alcohol intake, acute or chronic, while receiving Metformin.
Impaired hepatic function
Since impaired hepatic function has been associated with some cases of lactic acidosis, Metformin should generally be avoided in patients with clinical or laboratory evidence of hepatic disease.
Vitamin B12 levels
In controlled clinical trials of Metformin of 29 weeks duration, a decrease to subnormal levels of previously normal serum vitamin B12 levels, without clinical manifestations, was observed in approximately 7% of patients. Such decrease, possibly due to interference with B12 absorption from the B12-intrinsic factor complex, is, however, very rarely associated with anemia and appears to be rapidly reversible with discontinuation of Metformin of vitamin B12 supplementation. Measurement of hematologic parameters on an annual basis is advised in patients on Metformin of Metformin extended-release and any apparent abnormalities should be appropriately investigated and managed. Certain individuals (those with inadequate vitamin B12 or calcium intake or absorption) appear to be predisposed to developing subnormal vitaminB12 levels. In these patients, routine serum vitamin B12 measurements at two-to three-year intervals may be useful.
Change in clinical status of patients with previously controlled type 2 diabetes
A patient with type 2 diabetes previously well controlled on Metformin or Metformin extended-release who develops laboratory abnormalities of clinical illness (especially vague and poorly defined illness) should be evaluated promptly for evidence of ketoacidosis of lactic acidosis. Evaluation should include serum electrolytes and ketones, blood glucose and, if indicated, blood pH, lactate, pyruvate, and Metformin levels. If acidosis of either form occurs, Metformin of Metformin extended-release must be stopped immediately and other appropriate corrective measures initiated.
Hypoglycemia
Hypoglycemia does not occur in patients receiving Metformin of Metformin extended-release alone under usual circumstances of use, but could occur when caloric intake is deficient, when strenuous exercise is not compensated by caloric supplementation, or during concomitant use with other glucose-lowering agents (such as Sulfonylureas and Insulin) or ethanol. Elderly, debilitated, or malnourished patients, and those with adrenal or pituitary insufficiency or alcohol intoxication are particularly susceptible to hypoglycemic effects. Hypoglycemia may be difficult to recognize in the elderly, and in people who are taking beta-adrenergic blocking drugs.
Loss of control of blood glucose
When a patient stabilized on any diabetic regimen is exposed to stress such as fever, trauma, infection, or surgery a temporary loss of glycemic control may occur. At such times, it may be necessary to withhold Metformin and temporarily administer Insulin, Metformin may be reinstituted after the acute episode is resolved.
The effectiveness of oral antidiabetic drugs in lowering blood glucose to a targeted levels decreases in many patients over a period of time. This phenomenon, which may be due to progression of the underlying disease or to diminished responsiveness to the drug, is known as secondary failure, to distinguish it from primarily failure in which the drug is ineffective during initial therapy, combined therapy with Metformin of Metformin extended-release and Sulfonylurea may result in a response. Should secondary failure occur with combined Metformin/Sulfonylurea therapy of Metformin extended-release/Sulfonylurea therapy, it may be necessary to consider therapeutic alternatives including initiation of Insulin therapy.
-
សកម្មភាពឱសថ
Metformin is an antihyperglycemic agent which improves glucose tolerance in patients with type 2 diabetes, lowering both basal and postprandial plasma glucose. Its pharmacologic mechanisms of action are different from other classes of oral ant hyperglycemic agents. Metformin decreases hepatic glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing peripheral glucose uptake and utilization. Unlike Sulfonylureas, Metformin does not produce hypoglycemia in either patients with type 2 diabetes or normal subjects and does not cause hyperinsulinemia. With Metformin therapy, Insulin secretion remains unchanged while fasting Insulin levels and day-long plasma Insulin response may actually decrease.
*ព័ត៌មានឱសថត្រូវបានរៀបរៀងដោយ អ៊ីម៉ាតុគឹ មេឌីក (ខេមបូឌា) ដោយផ្អែកលើប្រភពព័ត៌មានខាងក្រោម។ សម្រាប់ព័ត៌មានលម្អិត សូមស្វែងរកនៅក្នុងក្រដាសព័ត៌មាននៃឱសថនីមួយៗ ឬ សាកសួរទៅកាន់ក្រុមហ៊ុនឱសថឬតំណាងចែកចាយនៃឱសថនីមួយៗ។
ប្រភពព័ត៌មាន៖
- ក្រដាសព័ត៌មាននៃឱសថសម្រាប់អ្នកជំនាញវេជ្ជសាស្ត្រដែលប្រើប្រាស់នៅប្រទេសជប៉ុន (Pharmaceutical and Medical Devices Agency, Pmda): https://www.pmda.go.jp
- ព័ត៌មានសង្ខេបនៃឱសថសម្រាប់អ្នកជំងឺដែលប្រើប្រាស់នៅប្រទេសជប៉ុន: http://www.rad-ar.or.jp
